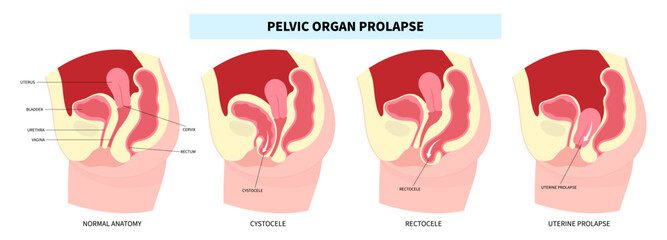
Urinary incontinence is characterized by involuntary leakage of urine due to the inability of the urinary system and/or pelvic floor to maintain urine in the bladder. There are different types of urinary incontinence:
- Stress incontinence
- Urge/urgency incontinence
- Mixed incontinence (stress and urge)
- Other rarer types
Despite popular belief in our society, urinary incontinence is not a “normal” condition due to aging or the effects of one or more pregnancies. With the right approach, urine leakage can be completely eliminated. Anyone suffering from incontinence should follow up with perineal rehabilitation. Trying to “solve” the problem with pantiliners or incontinence briefs is not a long-term solution. It’s never too late to address the problem.
It’s important to note that bladder weakness isn’t just a problem for women! In fact, it can occur in young athletes taking part in high-impact sports (gymnastics, trampoline, etc.) and in men. This condition is mainly found in men following surgery for prostate cancer (radical prostatectomy). Following prostate resection, 60% of men will experience urinary incontinence in the months following surgery. Refer to the radical prostatectomy blog for more info!
Stress Incontinence
Defined as urine leakage following a sudden increase in intra-abdominal pressure and the inability of the pelvic floor to keep the urethra closed. Most of the time, they will be triggered by coughing, sneezing, blowing the nose, laughing, jumping, etc. For most people, the leakage is due to
- Weak pelvic floor muscles → urethra not fully closed
- Lack of pelvic floor contraction (Knack) during exertion → urethra not closed at the right time
If you have these symptoms, here are a few tips:
- Physiotherapy assessment for perineal rehabilitation. Exercises and advice specific to your problem will be given to you.
- If you know how to do a pelvic floor contraction, try doing one before and during your triggers.
Urge/urgency Incontinence
Defined as urine leakage caused by overactive bladder muscles pushing urine out of the bladder. This type of incontinence is characterized by:
- A sudden, urgent urge to go to the toilet, followed by leakage
- Multiple visits to the toilet during the day
- Normal visits to the toilet = 6-8x/day
Unlike stress incontinence, it is often not caused by weak pelvic floor muscles, but rather by the bladder’s inability to stretch and accommodate urine normally. The bladder is “unhappy” and wants to get rid of urine immediately, even if it’s not full.
If you have these symptoms, here are a few tips:
- Physiotherapy assessment for perineal rehabilitation. Exercises and advice specific to your problem will be given to you.
- You can begin to apply the sequence of techniques for suppressing urges described below:
- Stop your activity. If there’s a seat nearby, it’s a good idea to sit down. The
sitting position increases your ability to retain urine. If no seat is available, remain still.
- Take deep breaths and try to relax.
- Try to motivate yourself. Examples:
- “I’m able to wait before going to the bathroom.”
- “I’m in control of the situation, not my bladder.”
- “My bladder isn’t really full, so it’s not urgent to go immediately.”
- Perform pelvic floor muscle contractions. You can choose the contraction parameters from the following 2 options:
- 2-3 sets of 8 fast, strong contractions
- 2-3 sets of one 8-second maximum contraction
- Do some mental work for 1 minute to take your mind off things. Examples:
- Count backwards from 100, name an object for each letter of the alphabet, name a to-do list (groceries, errands, other tasks)
- If the urge is still present, repeat steps 1 to 5
- When the urge is no longer pressing, but still present, go to the bathroom calmly and without hurrying. If the urge is gone, continue with your activities.
This strategy may take some time to become fully effective. The goal is to give you back control over your bladder. Be patient with the process. Practice will gradually make you better at controlling your urges.